|

|

|
causes and symptoms
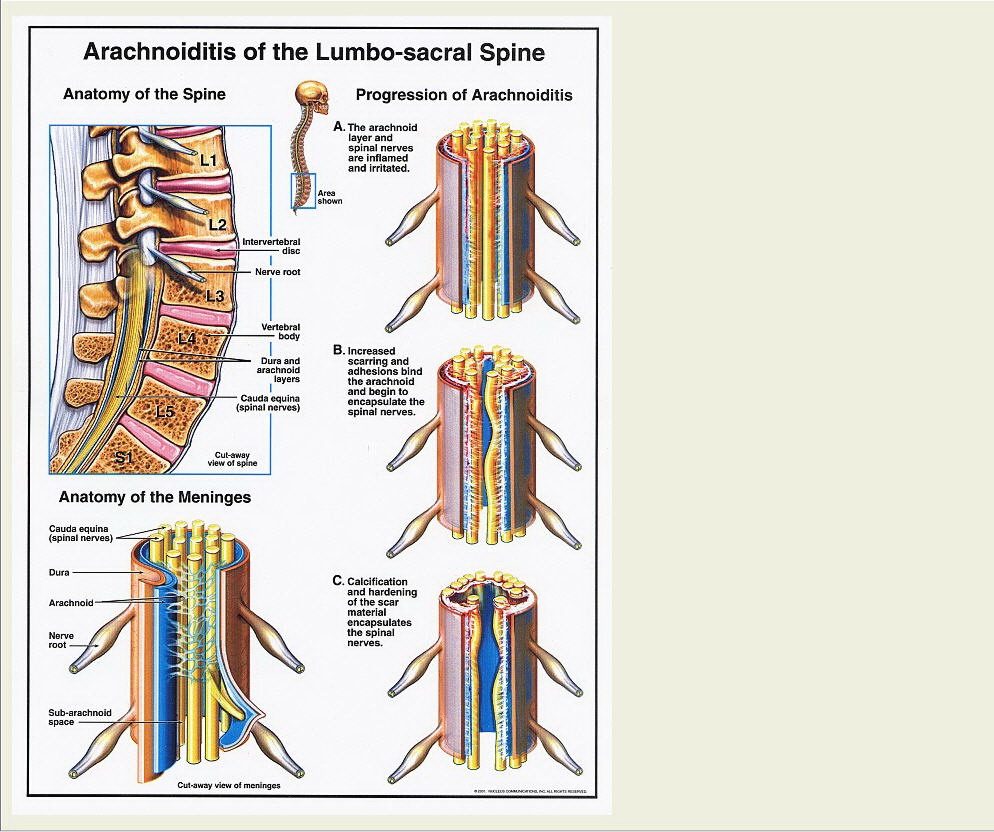
Arachnoiditis is a chronic inflammation of the arachnoid layer of the meninges, which are the coverings of the brain and spinal cord. The most severe form is Adhesive Arachnoiditis, which may be progressive.
The scarring produced by the disease causes many symptoms, the most debilitating of which is pain, typically constant and of a burning nature, sometimes with intermittent sharp, stabbing pains (sometimes described as electric shock sensation). The pain is principally in the lower back and limbs, although it may be found higher up the spine and radiate down the arms. Other sensory symptoms include:
Tingling or numbness
Heightened skin sensation
Normally painless stimuli may be painful
Strange sensations e.g. water running down leg.
Burning in ankles or feet; sensation like walking on broken glass
Movement (motor) functions may also be affected.
Symptoms include:
Weakness (rarely paralysis)
Muscle spasms
Muscle cramps
Bladder problems may also occur. These are due to involvement of the nerves that regulate bladder function, and may take one of two general forms: overactive bladder muscle causing urgency and incontinence, or under-active bladder, causing difficulty emptying the bladder, incomplete emptying and thus susceptibility to repeated infections. Similarly, the bowels may be affected.
Circulation in the extremities may be affected if the autonomic (involuntary) nervous system is involved. This system regulates functions such as blood vessel tone and there may be cold hands or feet, or possibly swelling (oedema).
From contacting numerous sufferers with arachnoiditis, it is becoming clear that there are often other symptoms, which may not at first glance appear related to the disease. These include:
Unexplained skin rashes
Joint and muscle pains (some patients have a dual diagnosis of fibromyalgia and arachnoiditis)
Heat intolerance
Cold chills/intermittent low-grade fevers
Difficulty swallowing
CAUSES:
Arachnoiditis has been known to the medical profession for many years as a rare complication of spinal surgery, trauma and meningitis (and other spinal infections such as TB).
However in more recent years, myelography has come under fire as a cause of this disease. You may well have heard of Myodil, which was banned. In America, there is now a Bill before Congress to ban the myelogram dyes, Pantopaque (oil-based) ,Amipaque, Omipaque and Isovue (water-based) as there is evidence to suggest that these dyes cause Arachnoiditis. Harry Feffer, Professor of Orthopaedic surgery at George Washington University states that patients who have had two or more myelograms stand a 50�hance of developing arachnoiditis.
More controversial still is the effect of epidural steroid injection. Depo-Medrol has been documented as being neurotoxic due to the benzyl alcohol that the steroid is suspended in. Manufacturers of several steroid preparations state that their use around the spine is contra-indicated. In Australia, legal action is being undertaken by about 100 people after treatment with Depo-Medrol. Dr. Charles Burton, At the Institute of low Back and Neck Care, Minnesota, states that “the most common foreign body causing adhesive arachnoiditis is Depo-Medrol” now that Iophendylate (i.e.Pantopaque) has been withdrawn from use. Whilst it is accepted by the medical community that “any foreign body substance introduced into the subarachnoid space has the potential of causing an inflammatory reaction (adhesions, arachnoiditis or adhesive arachnoiditis) “ (Charles Burton MD. 1997). The incidence of complications is still relatively low, which suggests that some patients have a predisposition to develop the more aggressive, uncontrolled reaction. More research needs to be done about this. There have been papers postulating a defective enzyme and there appears to be a possible autoimmune component. These are areas for further investigation.
DIAGNOSIS:
One of the most striking features of stories from patients with arachnoiditis is that they have nearly all had great difficulty obtaining a diagnosis. Many are told they have “Failed Back Surgery Syndrome” (FBSS). Charles Burton writes that “an international study…..has shown that lumbo-sacral adhesive arachnoiditis has been directly responsible for about 11�f all FBSS cases”.
Bearing in mind that arachnoiditis may be linked to a medical procedure, doctors may be reluctant to diagnose the disease. Also, there is at this time no known cure, but the disease is not generally life-threatening, so that practitioners may not want to give patients such a negative diagnosis. The first step in diagnosis, is, as always, a thorough history-taking and physical examination by the GP or hospital physician (usually a neurologist).
A high resolution MRI scan will help to exclude other causes, and may be useful in diagnosing arachnoiditis, especially if it is read by an experienced neuroradiologist. For bladder problems, a referral to an urologist for urodynamic testing may be necessary.
TREATMENT:
At this time, there is no definitive treatment for the disease process itself, although The Arachnoiditis Trust are setting up a working party of professionals to research the literature and establish international contacts with a view to getting research projects started. There are, however, various treatment modalities for the pain experienced, which tends to be the most debilitating factor. It is a “neurogenic” pain i.e. Generated by nerves, and as such is difficult to treat. Regimes include oral medication with anti-inflammatory agents; opioid drugs; adjuvant therapy with anticonvulsants and antidepressants, which are both very useful in this type of pain. This is not because there is a belief that the patient is either depressed or epileptic, and the drugs tend to be used at different doses to the ones used for depression or epilepsy. There are also other drugs to decrease muscle spasm. TENS machines may be of use, and may lead on to implantation of a spinal cord stimulator (which is like an internal TENS) for those patients who do not obtain good relief from drugs alone. In USA there are intraspinal narcotic pumps, but these may have serious side effects especially after prolonged use. Most encouragingly, there is a large body of research currently underway into a new class of drugs, which look very promising. Many patients suffer from the emotional effects of being in constant pain and the disabilities that this may impose upon them. These may be compounded by difficulties with the doctor/patient therapeutic relationship. However, referral to a specialist pain clinic may be useful in helping patients to gain an element of control over their illness. This can be very beneficial in improving the quality of life. Generally the pain management programmes tend to focus on cognitive/behavioural approaches i.e. using mental exercises to minimise the pain experienced, rather than using drugs, which may carry unacceptable side-effects. Sadly, many patients feel that referral to centres like this implies that they are not being taken seriously and that there is a suggestion that the pain is “in their head”. This is not to say that it is an issue of willpower, or that the patient is weak-willed or has a low pain threshold. Good doctors should take pains to reassure their patients that this is not the case. For some people, it can be a useful adjunct to other therapy.
Dr Sarah Fox
@ASAMS New Zealand
|
|