|
cerebro spinal Fluid Leak
Cerebrospinal fluid depletion may be caused by a leak, a shunt, inadequate production or too rapid absorption.
Symptoms commonly include headaches, which are more severe in the upright position and are alleviated by supine or head-lowered below chest(Trendelenburg) positioning. There may also be nausea and tinnitus. Horizontal diplopia, change in hearing, tinnitus, blurring of vision, facial numbness and upper limb radicular symptoms (tingling) may occur. These symptoms are nonspecific as they are commonly encountered in migraine and post-traumatic headache. Cognitive decline has also been reported (Hong et al, 2002; Pleasure et al, 1998).
As this is an otoneurology site, we will go into the hearing related symptoms in a bit more detail. While CSF leak is generally accompanied by an orthostatic (upright only) headache, this association is not universal and in fact, hearing loss may be more common than headache (Oncel et al, 1992). Orthostatic tinnitus is also possible.(Arai, Takada et al. 2003). The hearing loss of CSF leak likely results from lowering of CSF pressure, which lowers perilymphatic (inner ear) pressure, and results in a picture similar to Meniere's disease. (Walsted et al., 1991).
Locations of CSF leaks
The leaks are typically at the level of the spine, particularly the thoracic spine and cervicothoracic junction. Sometimes they are unintentional consequences of an overdraining CSF shunt (e.g. VP shunt), placed for CSF hypertension (hydrocephalus). They can follow spinal surgery (Sin, 2006). CSF leaks can also occur in the ear through weaknesses in the roof of the middle ear, as well as from the nose after trauma or surgery.
Sinus surgery and pituitary surgery are the main sources of leaks through the nose. The "Dandy maneuver" -- bending forward, and straining to see if this produces clear nasal discharge, can be used to diagnose these types of leaks if they are large ones.
CSF leaks may follow diagnostic or therapeutic lumbar puncture as well as spinal anesthesia and after an inadvertant puncture of the dura following epidural anesthesia or epidural steroid injections (Johkura et al. 2000). In this case, the leak is at the site of the puncture. Symptoms from the leak can be delayed for as long as a month (Lybecker and Anderson, 1995). It seems likely that these cases are often missed.
Movie of CSF pulsations in ear tube(1,5 meg) (From Richard Wiet, M.D.)
CSF leaks into the middle ear are probably rare, although large numbers have been reported (Leonetti et al, 2005). The leaks can be acquired, congenital or spontaneous. Acquired leaks can be caused by head injury, surgery, infection or tumor. Congenital leaks are most often associated with the development of anomalous transcranial pathways. CSF leaks into the middle ear are accompanied by serous otitis.
Spontaneous leaks into the middle ear are usually diagnosed by high-resolution CT scans. This may reveal discrete tegmen defects, multiple pinhole fistulae, or a combination of these findings. About 6f the population has some degree of bony defect. Most patients have an ipsilateral conductive or mixed hearing loss, the conductive component caused by CSF in the middle ear. These can be repaired via a middle fossa craniotomy (Leonetti et al, 2005).
A ventilation tube should not be put into an ear with a CSF leak, as this might provide a route for infection to enter the brain.
To be sure that there is no CSF leak, one would need to do a high-resolution temporal bone CT scan in every person with otitis media with effusion. At this writing, perhaps because of the rarity of CSF leaks, this is not generally done. Instead, if continuous drainage of clear fluid is noted through the ventilation tube (as shown above), this observation leads to the diagnosis of a CSF leak from the ear. The video above (courtesy of Dr. R. Wiet, who was referred this patient with the tube in place), shows CSF pulsating in a ventilation tube.
Spontaneous leaks
Spontaneous leaks from the nose are somewhat uncommon (1/26 in Mokri, 1997). Speculatively, it would seem possible that CSF leaks might occur after whiplash injury, as frequently there are persistent similar symptoms without findings on other studies. CSF leaks have been reported due to cervical bone spurs (Miyazawa et al, 2003; Vishteh, Schievink et al. 1998). At this writing however (2002), almost nothing has been published regarding this possibility.
Other things that can look like a leak
Other conditions to exclude when considering the diagnosis of CSF leak are orthostatic hypotension (which can cause dizziness on standing), positional vertigo due to inner ear disturbances such as BPPV, and orthostatic tremor. When considering leaks from the nose, of course other fluids than CSF can leak out of the nose. "Pseudo-CSF rhinorhea" can occur as a result of injury to the sphenopalatine ganglion (Hilinski et al, 2001).
CSF leaks can also result from high-pressure hydrocephalus. In this situation, leaks may recur until the cerebral ventricles are shunted (Tosun et al, 2003)
Diagnostic testing
Tests requiring lumbar puncture:
On lumbar puncture, in approximately half of patients, the opening CSF pressure is 40 mm or less. However, if this is found, one still needs to locate the site of leak. The other half of patients may have normal CSF pressure so a lumbar puncture is not 100eliable to diagnose low CSF pressure. Of course, there is some danger of causing a leak, per se, with a lumbar puncture, and the risks/benefits must be carefully considered. In a small minority of patients with CSF leak, CSF pressure may be normal although patients continue to have symptoms and abnormal MRI findings. Perhaps this indicates an intermittent situation.
In the past it was thought that CSF could be distinguished from other fluids by it's glucose content. Testing of the fluid dripping from the nose for glucose is no longer thought to be useful. Testing for beta-transferrin may help determine if it is CSF or something else.
A surer method is to inject radioactive label or a fluorescent dye into the spinal fluid and test for the label or dye in the fluid. Nasal pledgets can be left in the nose for extended periods, enabling detection of intermittent rhinorhea. 0.5 ml of 5luorescein diluted in 9.5 cc of CSF is used (according to Hilinski et al, 2001). Smaller amounts are used in children. (Lue and Manolidis 2004). It is useful to use control pledgets under the upper lip for comparison. the test is analyzed under ultraviolet light. No complications were reported by Montgomery in more than 200 injections of fluorescein. However some authors have reported seizures from fluorscein can occur.
Radioactive label materials may include technetium or indium 111. Indium is an agent that attaches specifically to CSF proteins. A major disadvantage of the radioactive imaging is high cost and the possibility of false-positive results. This study requires injection of material into the spinal canal, a process which could introduce a CSF leak by itself.
Radiologic studies are also useful -- CT contrast cisternography after metrizamide injection is considered to be the most useful during a leak. This may be impractical however if one does not know the level of the leak and can also be falsely localizing (Lue and Manolidis 2004).
Radioisotope cisternography characteristically shows a decrease or absence of activity over the cerebral convexities and early accumulation of radioisotope in the bladder. This study is somewhat invasive, requiring injection of material into the spinal canal.
Gadolinium MRI documenting location of CSF leak (arrow). Image from Jinkins et al, 2002.
A new test, injection of a small amount of gadolinium contrast into the lumbar spinal fluid followed by MRI is very promising (Jinkins et al, 2002). Gadolinium is non-toxic as is CT contrast dye, and also while CT contrast could be confused with bony structures, gadolinium is not easily confused with other body parts. Of course, MRI can scan the entire neuroaxis if the site of leak is unclear. In our practice in Chicago, we obtain this test using a facility in Morton Grove Illinois (a suburb of Chicago).
Spinal fluid testing may show a minor pleocytosis of 5 or more cells, and a modest and variable increase in protein (Mokri et al, 1997).
Tests not requiring lumbar puncture:
Before starting the discussion, lets first say that none of these techniques are very useful. The best, at the present time, involves using MRI to find side effects of low CSF pressure -- venous engorgement or downward displacement of the brain.
Head MRI findings include diffuse meningeal gadolinium enhancement due to engorgement of the cerebral venous system (Mokri et al, 1997), imaging evidence of sinking of the brain resembling the Chiari malformation (Paynor, 1994), subdural fluid collection, decrease in ventricular size and prominent dural sinuses. Spine MRI may show extra-arachnoid fluid, meningeal diverticuli, meningeal enhancement, or engorgement of epidural venous plexi (Miyazawa et al, 2003). The engorgement of the epidural venous plexus is analogous to the findings on cerebral MRI. This finding may be missed if the MRI is read by a radiologist unfamiliar with this syndrome.
Recently it has been reported that doppler or MRI of the superior opthalmic vein may reveal abnormalities in persons with low CSF pressure (Chen et al. 1999; Chen et al., 2003). Doppler may show increased flow velocity. It may be difficult to find a sonographer with expertise in this method. We have not tried to use this method in Chicago -- and it also seems unlikely to work in any case.
MRI may show collapse of the superior opthalmic vein (Chen et al., 2003). Radiologists do not generally measure the diameter of the superior opthalmic vein, and if this technique is planned, it seems prudent to either seek out an experienced radiologist or develop the expertise through a series of MRI's done in normal persons. We have not had any success in this technique to date, but this may be simply because we have not seen an appropriate patient.
Leaks of spinal fluid from the nose or external ear can be detected by assaying the fluid with a new test called beta-trace protein assay (Bachman et al, 2002; Wernecke et al, 2004). It is too soon to say if this test will become widely available and useful. It is our thought that if there is so much fluid that it you can see it leaking in front of your eyes, you should use one of the spinal fluid tests instead.
Audiometry (hearing testing) is sometimes affected by CSF-leak. (Kilickan and Gurkan, 2003) The pattern of hearing loss may resemble that of Meniere's disease. Although logically, hearing should improve in the supine position, this has been little studied. We are presently studying a protocol involving changes in OAE's with position in our clinic. At this writing, it is too soon to know if it is useful.
Treatment
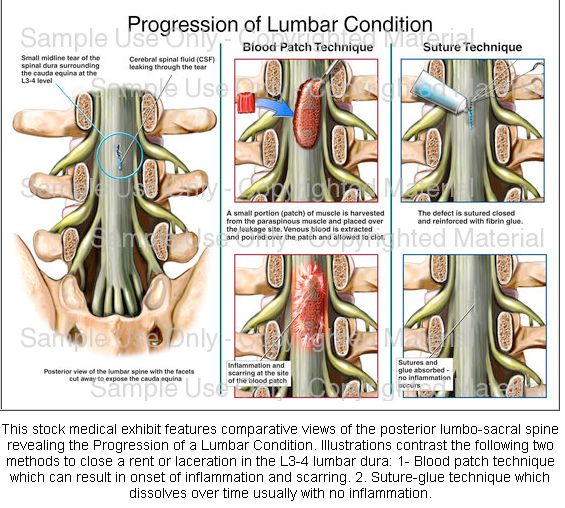
Treatment may include bed rest, hydration and steroids. Epidural blood patch is used in patients with spinal leaks who fail noninvasive measures. Blood patches are generally thought to be safe but occasional reports of increased CSF pressure and persistent epdurual fluid collections have been reported. Surgical repair is used in patients with leaks in the skull.
The overwhelming majority of patients have a spinal level leak, although they are generally higher than the lumbar level (Mokri, 1997). Surgical repair may be performed in patients that fail blood patch if the site of the leak has been identified.

REFERENCES:
Bachman and others. Incidence of occult cerebrospinal fluid fistula during perinasal sinus surgery. Arch Otol HNS, 2002, 128, 1299-302
Chen CC, Luo CL, Wang SJ, Chern CM, Fuh JL, Lin SH and Hu HH (1999). "Colour doppler imaging for diagnosis of intracranial hypotension." Lancet 354(9181): 826-9.
Chen WT, Fuh JL, Lirng JF, Lu SR, Wu ZA and Wang SJ (2003). "Collapsed superior ophthalmic veins in patients with spontaneous intracranial hypotension." Neurology 61(9): 1265-7.
Hilinski JM, Kim T, Harris JP. Posttraumatic pseudo-cerebrospinal fluid rhinorhea. Otol Neurotol 22:701-05, 2001
Hong M, Shah GV, Adams KM et al. spontaneous intracranial hypotension causing reversible frontotemporal dementia. Neurology 2002:58:1285-87
Jinkins JR, M Rudwan, MD, G Krumina, and E. Tali. Intrathecal Gadolinium-enhanced MR Cisternography in the Evaluation of Clinically Suspected Cerebrospinal Fluid Rhinorrhea in Humans: Early Experience. Radiology 2002;222:555-559.
Johkura, K., Y. Matsushita, et al. (2000). "Transient hearing loss after accidental dural puncture in epidural block." Eur J Neurol 7(1): 125-6.
Kilickan, L., Y. Gurkan, et al. (2003). "The effect of combined spinal-epidural (CSE) anaesthesia and size of spinal needle on postoperative hearing loss after elective caesarean section." Clin Otolaryngol 28(3): 267-72.
Leonetti JP and others. Spontaneous transtemporal CSF leakage: A study of 51 cases. ENT J. 84:11, 700-706, 2005,
Lue, A. J. and S. Manolidis (2004). "Intrathecal fluorescein to localize cerebrospinal fluid leakage in bilateral Mondini dysplasia." Otol Neurotol25(1): 50-2.
Lybecker, H. and T. Andersen (1995). "Repetitive hearing loss following dural puncture treated with autologous epidural blood patch." Acta Anaesthesiol Scand 39(7): 987-9.
Miyazawa K and others. CSF hypovolemia vs intracranial hypotension in "spontaneous intracranial hypotension syndrome". Neurology 2003:60:941-947
Mokri B, Piepgras DG, Miller GM. Syndrome of orthostatic headaches and diffuse pachymeningeal gadolinium enhancement. Mayo Clin Proc 1997:72:400-413
Mokri B, Atkinson JLD. False pituitary tumor in CSF leaks. Neurology 2000:66:573-575
Mokri B, Posner JB. Spontaneous intracranial hypotension. The broadening clinical and imaging spectrum of CSF leaks. Neurology 2000:55:1771-1772
Montcomery WW. repair of dural defects. In Surgery of the upper respiratory system, 2nd ed, Vol 1, Philadelphia: Lea and Febiger, 1979
Oncel, S., L. Hasegeli, et al. (1992). "The effect of epidural anaesthesia and size of spinal needle on post-operative hearing loss." J Laryngol Otol 106(9): 783-7.
Payner TD, Prenger E, Berger TS, Crone KR. Acquired Chiari malformations: incidence, diagnosis, and management. Neurosurgery 1994;34:429-434; discussion 434.
Pleasure Sj and others. Spontaneous intracranial hypotension resulting in stupor caused by diencephalic compression. Neurology 1998:50:1854-57
Sin AH, Caldito G, Smith D, Rashidi M, Willis B, Nanda A. Predictive factors for dural tear and cerebrospinal fluid leakage in patients undergoing lumbar surgery. J Neurosurg Spine 2006;5:224-227.
Tosun F, Carrau RL, Snyderman CH, Kassam A, Celin S, Schaitkin B. Endonasal endoscopic repair of cerebrospinal fluid leaks of the sphenoid sinus. Arch Otolaryngol Head Neck Surg 2003 May;129(5):576-80
Vishteh AG, Schievink WI, Baskin JJ and Sonntag VK (1998). "Cervical bone spur presenting with spontaneous intracranial hypotension. Case report." J Neurosurg 89(3): 483-4.
Warnecke A and others. Diagnostic relevance of beta-2 transferrin for detection of cerebrospinal fluid fistulas. Arch Otolaryngol Head Neck Surg; 130:1178-1184
|